Denture Replacement and Aging: What Changes in Your Mouth Over Time

Table of Contents
- Signals to Look for in Denture Replacement
- Why Denture Fit Gets Worse as You Age
- Other Common Oral Issues in Older Adults
- What You Can Do to Protect Your Smile as You Age
- Why Denture Replacement Matters for Overall Health
- What to Ask Your Dentist at Your Next Visit
- Family Checklist: Oral Health Questions for Long-Term Care Facilities
As you get older, maybe reaching your 60s, 70s, or beyond, you probably notice the usual signs of aging: skin that sags, joints that creak, and strength that fades a bit. But your mouth changes too. Teeth shift. Gums recede. Bones shrink. That can create trouble for dentures — and for your overall oral health.
Here’s what you should know about how often dentures need replacing, and which age-related oral problems affect many older adults. Be sure older family members are adding oral health and if they live in a long-term care facility be sure the staff is watching for oral health issues as part of their care plan.
Typical Denture Lifespan: Know When It’s Time for New Ones
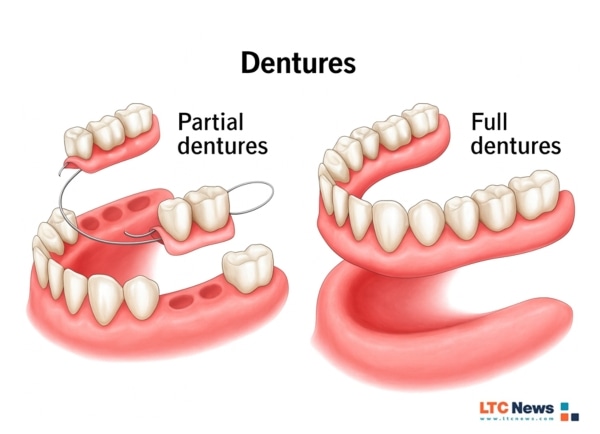
Most removable dentures, full or partial, have a useful lifespan. According to experts, dentures tend to last about 5 to 10 years on average.
More specifically:
- Some dentists recommend that full dentures be replaced every 7 to 10 years.
- Others note that many dentures may need replacement after 5 to 7 years, depending on wear, material, and how well they were cared for.
- Partial dentures (when you still keep some natural teeth) sometimes last longer — up to 10–15 years — but that depends a lot on how your jaw and gums change over time.
Even with diligent care, including good cleaning, occasional relines, and proper storage, dentures eventually wear out or stop fitting well.
Dentists often perform a “reline” (reshaping the base to match changing gums or bone) every 1–2 years to keep dentures comfortable, but that doesn’t replace the need for new dentures down the road.
Signals to Look for in Denture Replacement
If you notice any of the following, the American College of Prosthodontists says it’s time to check with your dentist about the replacement of your dentures:
- Dentures feel loose, slip, or shift when you eat, speak, or laugh.
- Chronic irritation, sore spots, or gum pain under the dentures.
- Broken, cracked, or discolored teeth or denture base.
- Difficulty chewing or speaking clearly.
- You need denture adhesive more than occasionally to keep them in place.
Why Denture Fit Gets Worse as You Age
A big reason dentures become less comfortable over time is due to the structural changes in your mouth.
- When natural teeth are lost, the jawbone slowly resorbs (shrinks) — a normal process that continues over years. That changes the shape of your mouth and gums, so dentures that once fit snugly may become loose.
- As gum tissue and bone shrink, dentures may shift or rock when you bite or talk. That instability can irritate gums and lead to sores or even infections.
- Wear and tear: everyday chewing, biting, and even cleaning contribute to the deterioration of denture materials over time — especially the acrylic base or prosthetic teeth.
Because of these changes, even the best-maintained dentures eventually wear out or stop fitting properly.
Other Common Oral Issues in Older Adults
Even if you don’t wear dentures, aging can bring oral health issues that many people don’t expect. Some that become more common with age:
Tooth Discoloration
Enamel naturally becomes thinner over decades, exposing more of the yellowish dentin beneath. Coffee, tea, wine, tobacco, and certain foods accelerate staining. Whitening treatments are popular — but older adults may more often experience sensitivity or gum irritation, especially if enamel is thin or gums have receded.
Gum Recession and Gum Disease
Gums tend to recede with age; medications, chronic dry mouth, or reduced saliva flow increase the risk of gum disease. Pockets can form where bacteria accumulate, exposing sensitive roots and increasing the risk of decay or infection. If your teeth feel sensitive to temperature changes or pressure, it could be a sign that you need a procedure like a root canal because they can no longer protect the nerve inside from stimuli.
Wear, Cracks, and Brittleness in Teeth
Lifelong chewing, grinding, and biting wear down enamel. Over time, cracks or “hairline fractures” can form, leaving teeth vulnerable to breaking or root exposure — which may lead to pain, increased sensitivity, or infection.
Dry Mouth & Reduced Saliva Production
Many older adults take medications that reduce saliva. Since saliva helps wash away food debris and neutralize acids, reduced saliva flow increases the risk of cavities, enamel erosion, and gum problems.
Tooth Loss, Bone Loss, and Jawbone Shrinkage
Advanced gum disease, decay, or years of wear can lead to tooth loss. Without the stimulation from natural tooth roots, the jawbone may gradually shrink — altering facial structure, making chewing harder, and destabilizing dentures or other dental appliances.
What You Can Do to Protect Your Smile as You Age
You can’t stop aging — but you can slow or reduce oral problems with good habits and regular care. Try these:
- Keep brushing at least twice a day and floss daily (or use interdental cleaners). Good hygiene delays enamel wear, gum disease, and tooth loss.
- If you have dentures, the Cleveland Clinic and ADA suggest removing them nightly, cleaning them using a soft brush, and soaking them overnight in a denture cleanser (not regular toothpaste).
- Visit your dentist regularly (at least once a year; more often if you wear dentures). Dentists can check fit, clean your gums, look for early signs of decay or gum disease — and reline or adjust dentures as needed.
- Mention any discomfort, soreness, or ill fit immediately. Don’t wait until it becomes painful or you stop wearing your dentures comfortably.
- Consider whether a more stable solution — such as implant-supported dentures or overdentures — might work better as your bone structure changes.
Why Denture Replacement Matters for Overall Health
Wearing dentures that no longer fit or have deteriorated might not just be a comfort issue. According to the position statement of the American College of Prosthodontists (ACP), old or degraded dentures can harbor bacteria, fungi, and other pathogens that accumulate in microscopic porosities of the denture base. That can lead to oral inflammation, infection, and even contribute to respiratory problems such as pneumonia.
Replacing dentures on the right timetable isn’t just cosmetic, it’s about preventing serious health issues.
What to Ask Your Dentist at Your Next Visit
- Do my dentures still fit properly? If not, should they be relined or replaced entirely?
- Are there signs of gum disease, recession, or bone loss that could affect denture fit or my remaining teeth?
- Could an implant-supported denture or overdenture be a better long-term solution for me?
- Any recommendations to reduce dry mouth, improve saliva flow, or protect enamel?
- How often should I come in for cleanings or check-ups now that I’m older?
How Oral Health is Managed in Long-Term Care — What Families Should Ask
Older adults living in assisted living and nursing homes rely on caregivers to manage their daily hygiene, including dentures, brushing, and mouth care. When facilities are understaffed or aides are rushed, oral care is often skipped or done superficially.
The result can be painful infections, poor nutrition, and a faster decline in overall health. Asking questions and monitoring your loved one’s mouth care helps ensure their comfort and safety.
Family Checklist: Oral Health Questions for Long-Term Care Facilities
Daily Care
- How often is my loved one’s mouth cleaned each day?
- Who is responsible for oral hygiene (nurse or aide)?
- Are staff trained in cleaning dentures and natural teeth?
- If they resist brushing due to dementia, how is that handled?
Denture Care
- Are dentures removed and cleaned every night?
- Are dentures stored in a sealed, labeled container?
- Is the fit checked regularly to prevent sores and chewing problems?
- Who should I speak with if my loved one complains about pain or discomfort?
Monitoring and Documentation
- Will oral pain, sores, or cracked dentures be documented and reported to me?
- Is weight loss ever evaluated for possible dental or denture causes?
- How does the staff manage dry mouth caused by medications?
- Is there a schedule for oral assessments? How often?
Access to Dental Providers
- Does the facility have a dentist who makes on-site visits?
- If not, how are dental appointments arranged and transported?
- How quickly can my loved one be evaluated if a problem appears?
When moving an older family member to a long-term care facility, ask these questions as part of your facility research.
Use the LTC News Caregiver Directory to start the process of finding quality caregivers and long-term care facilities in any zip code in the United States. If your loved one has Long-Term Care Insurance be sure to tell the admission’s manager that the policy exists. Having an LTC policy can help secure your loved one a space at a better facility. Remember that Medicare only pays for short-term skilled care, not for most long-term care services.
👉 Need help filing a claim? LTC News partners with Amada Senior Care to provide free claim support with no cost or obligation. Their trained experts can walk you through the entire process and help you access benefits quickly and correctly — File a Long-Term Care Insurance Claim. If there is no LTC policy, and your loved one has a life insurance policy, you could sell it for cash now to cover the costs of care.
Aging might bring more oral health challenges, but it doesn’t mean you have to settle for slipping dentures, discomfort, or a fading smile.
With good hygiene, regular dental check-ups, and timely denture replacement or upgrades, you can still enjoy comfort, function, and confidence in your smile.


