Addiction Doesn’t Retire: Substance Misuse After 60

Table of Contents
- Late-Life Addiction is Real, Common, and Often Missed
- Prescription Drugs: The Hidden Driver After 60
- Alcohol And Retirement: When A Routine Becomes Risky
- Why Families and Healthcare Professionals Miss the Signs
- Warning Signs That Deserve a Closer Look
- Stigma Around Addiction in Seniors
- The Elder Abuse Link: How Harm Develops at Home or in Care
- If You Suspect Abuse, Speak Up and Report
- Grief and Loneliness Are Common Triggers
- Talk Early About Addiction. Talk Kindly. How To Start
You want your later years, or your parents’ years, to feel steady and safe. Maybe you picture family dinners, travel, a slower pace, or simply feeling secure at home. What most people do not picture is addiction.
It is not the image that comes to mind when you think of a retired grandparent, a loved one in their seventies, or even yourself. Addiction does not age out. It does not disappear once you get your AARP card. Addiction does not care if someone has raised a family, built a career, or survived life’s toughest storms.
For many older adults, substance misuse does not look like parties or street drugs. It creeps in through quiet routines. A couple of drinks each night. A sleeping pill to get through the night. Pain medicine after a surgery that never quite gets tapered. It slips under the surface, hidden by normal aging, loneliness, or grief.
In fact, late-life addiction and just senior addiction in general are far more common than people realize. You may not notice it at first. Your loved one may not either. By the time it is visible, the harm is more than physical. It touches dignity, independence, and the sense of safety every older adult deserves.
If you are worried that something is not quite right with a parent, spouse, or even yourself, you are not alone. Addiction among older adults is far more common than most people realize. It can speed health decline, make aging at home unsafe, and increase the need for care. Most importantly, it can be addressed. With understanding, the proper support, and early action, recovery is possible at any age.
Late-Life Addiction is Real, Common, and Often Missed
Older adults take more medicines and live with more chronic pain than younger people. That raises the risk for dependency and dangerous drug interactions.
National survey data confirm that millions of people in the United States report substance use each year. The 2024 National Survey on Drug Use and Health summarizes key indicators and trends that clinicians and policymakers use.
Falls and overdoses show the stakes. CDC reporting and national coverage highlight rising fall deaths among older adults and ongoing concerns with drug harms in people 65 and older. These patterns point to gaps in screening, medication review, and coordinated care.
Why it matters: Substance misuse raises the risk of falls, hospital stays, cognitive decline, and the need for long-term care services. These events can trigger sudden needs for help with activities of daily living and/or supervision due to cognitive decline. These daily needs include things we take for granted, like personal hygiene, bathing, dressing, and medication management.
Prescription Drugs: The Hidden Driver After 60
As you age, pain, sleep problems, and anxiety are common. Prescriptions help. One of the most significant contributors to addiction in older adults is sitting right in plain sight: prescriptions. You’re probably already familiar with the opioid epidemic that’s specifically happening in the Appalachian region of the United States; however, it’s spreading throughout the country and worldwide.
Dependence can creep in quietly, especially with opioids, benzodiazepines, and sedative-hypnotics.
So, as people age, medications pile up: pain management, sleep aids, anti-anxiety meds, muscle relaxants, you name it. Doctors prescribe them to help, and often they do. But dependency can build slowly, sometimes so subtly that no one notices until it’s become a real issue. But unlike recreational drug use, prescription dependency often looks almost “normal.”
- The American Geriatrics Society’s Beers Criteria list medicines that are potentially inappropriate for older adults because risks can outweigh benefits. Benzodiazepines and several sleep medicines appear on this list.
- A 2025 Substance Abuse and Mental Health Services Administration (SAMHSA) letter urges healthcare providers to reduce chronic benzodiazepine use in older adults when possible because of higher risks, including falls, fractures, delirium, and cognitive impairment.
Older adults who take benzodiazepines are at greater risk of adverse events than younger patients, including falls and hip fractures, motor vehicle collisions, delirium and cognitive impairment. — SAMHSA Dear Colleague Letter, June 5, 2025.
What you can do: Ask for a complete medication review for your older loved one. Bring every bottle. Request non-drug approaches for sleep or pain when appropriate. If a medicine needs to be stopped, follow a supervised taper under your doctor's supervision. Johns Hopkins offers a plain-language overview of how alcohol and medicines affect older adults.
Alcohol And Retirement: When A Routine Becomes Risky
A nightly drink can turn into several. Loneliness, grief, and boredom make that slide easy. The National Institute on Alcohol Abuse and Alcoholism notes that alcohol-related harms are rising among older adults, with faster increases among women.
The CDC’s message is simple. Drinking less is better for your health than drinking more. Choosing to drink less lowers health risks and injury risk.
Family tip: Notice patterns in older adults. Is the pour larger? Are social drinks becoming solitary? Gentle questions can open a safer conversation.
Why Families and Healthcare Professionals Miss the Signs
The symptoms can look like normal aging. Memory slips, daytime sleepiness, mood swings, and balance problems can come from alcohol or medicines. They can also come from other illnesses.
That overlap hides problems in plain sight. Falls remain the leading cause of injury for adults 65 and older. Screening for medicines and alcohol is part of fall prevention.
Watch for combinations: Alcohol with sedatives. Opioids with sleep aids. Multiple prescribers. Early refills. Unexplained falls.
Warning Signs That Deserve a Closer Look
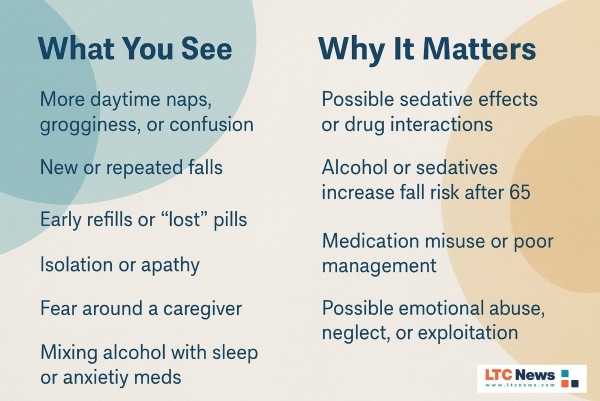
These patterns often look like aging. They may be treatable signs of substance misuse or abuse. Use them to guide a supportive, safety-focused conversation.
Stigma Around Addiction in Seniors
Stigma is one of the biggest reasons addictions among older adults often goes unnoticed. It’s easier for families to acknowledge substance use problems in teenagers or young adults.
But when it’s someone’s parent or grandparent, denial can run deep. Families may not want to believe it, seniors may not want to talk about it, and the topic is often pushed aside.
That silence can make the problem worse. Addiction thrives in isolation, and many older adults already struggle with loneliness. Add shame into the mix, and it becomes even harder to reach out for help.
The idea that treatment is only for young people is simply wrong. Professional care is just as essential and sometimes even more critical for older adults.
Many unique challenges make senior recovery different from recovery in younger adults. And that’s why involving experts can be life-changing.
Sometimes this means exploring counseling, sometimes it means finding community support groups, and sometimes it means turning to an addiction recovery center that understands how to tailor treatment to seniors.
But for struggling seniors, there absolutely needs to be the proper structure and guidance in place, and stigma shouldn’t get in the way of reaching out for help.
The Elder Abuse Link: How Harm Develops at Home or in Care
Substance misuse and elder abuse can intersect. Alcohol or sedative use can increase a senior’s vulnerability to neglect or financial exploitation.
Caregivers can also be affected by the physical and emotional demands of caring for a loved one. Even professional caregivers can experience this strain.
Caregiver stress, untreated mental health issues, and dependence can also raise the risk that a caregiver becomes an abuser.
- CDC defines abuse of older persons as an intentional act or failure to act by a caregiver or trusted person that causes harm or risk of harm. Types include physical, emotional, sexual, financial exploitation, and neglect.
- The National Center on Elder Abuse provides training, research, and practical tools for families and professionals.
- Risk factors exist at the individual, relationship, community, and societal levels. Understanding these factors helps with prevention and early intervention.
There are several things a family member may notice. Unexplained bruises. Sudden money changes. Poor hygiene. Missed medicines. Isolation or fear around a caregiver. NCEA and partner fact sheets list common red flags and steps to take.
How it can start: A son managing bills during a parent’s recovery begins controlling accounts. A stressed spouse with back pain mixes alcohol with pills and neglects care tasks. A facility short on staff misses hydration and turning schedules. Small safety lapses grow into patterns that cause harm.
What helps: Remove access to finances when exploitation is suspected. Rotate caregiving duties. Bring in outside help. Use respite care. Consider a change in care setting if safety cannot be restored.
If You Suspect Abuse, Speak Up and Report
Sometimes an older adult or caregiver with an addiction may abuse an older spouse. If someone is in immediate danger, call 911. The Department of Justice Elder Justice Initiative explains how to find help or report abuse in your state.
For non-emergencies, contact Adult Protective Services in the state where the person lives. The Administration for Community Living and NCEA provide state reporting resources. You can also call the Eldercare Locator at 1-800-677-1116 to connect with local services.
Financial crimes and scams are common. The National Elder Fraud Hotline at 833-FRAUD-11 offers case management and help with reporting.
Grief and Loneliness Are Common Triggers
One of the most challenging realities of aging is the wave of life changes that often come with it. Losing a partner, saying goodbye to lifelong friends, downsizing to assisted living, or facing health challenges that limit your independence can leave you feeling unmoored. These experiences aren’t just painful — they can reshape your entire sense of self.
When grief and loneliness weigh heavily, many older adults turn to unhealthy coping mechanisms, including substance use, to ease the pain. But those temporary escapes can deepen the isolation, creating a cycle that’s hard to break.

Share your thoughts and experiences about aging, caregiving, health, retirement, and long-term care with LTC News —Contact LTC News.
Without meaningful support, what begins as a way to cope can quietly grow into something far more dangerous. Older adults who are lonely and grieving often benefit from consistent social connections and compassionate, quality care.
Having professional caregivers in the home can provide both emotional support and daily assistance. In assisted living communities, regular social activities and shared experiences can ease isolation and help your loved one feel more connected, ultimately improving their overall quality of life.
👉 You can use the LTC News Caregiver Directory to find long-term care facilities and home care agencies in your area. Search quality providers allows you to compare not just services, but also how they support residents who are grieving or feeling lonely. You should also ask how they help prevent and handle addiction.
If your loved one has Long-Term Care Insurance, be sure to tell the provider that a policy exists. LTC News partners with Amada Senior Care to provide free claim support with no cost or obligation. Their trained experts can walk you through the entire process and help you access benefits quickly and correctly — File a Long-Term Care Insurance Claim.
Visit the LTC News Education Center for planning guides, numerous tools, and resources.
Talk Early About Addiction. Talk Kindly. How To Start
Open with concern, not accusation. Keep it short and specific.
- “I noticed a few new falls and extra sleepiness. Can we review medicines with your doctor together.”
- “You used to have one drink. It seems like it is more now. How are you sleeping.”
- “Would you try a bedtime routine or physical therapy instead of another pill.”
Ask the primary care doctor about screening, deprescribing, pain alternatives, and a referral to geriatric medicine or addiction care.
This article is intended for information only. It is not medical advice. Speak with your doctor about your situation.


