Spotting Institutional Abuse in Long-Term Care: How to Speak Up and Take Action

You made a hard, loving choice when you placed your mom, dad, spouse, or even a younger family member with special needs in extended care. Most caregivers are compassionate professionals doing difficult work under pressure. Don’t assume, though.
Problems hide in plain sight, and vulnerable people don’t always tell you when something’s wrong. Your attention is protection.
What “Institutional Abuse” Means — Why it’s Hard to See
Institutional abuse is harm caused by people, policies, or practices inside a care setting — nursing homes, assisted living, memory care, group homes, psychiatric units, or youth residential programs.
Like elder abuse, cases involving youth transition campus sexual abuse have shown how long-term mistreatment can remain hidden for years, with warning signs either missed or dismissed. Situations like these underscore the need for early recognition and consistent monitoring.
It can be physical, emotional, sexual, financial, or neglect — and often more than one at once. People who depend on others for basic needs are at higher risk, and cases are frequently missed or minimized.
Research from the World Health Organization indicates that elder abuse is common in institutions, with two in three staff reported perpetrating some form of abuse in the past year.
Why it’s missed: cognitive impairment blurs stories, fear of retaliation silences residents, and families may get vague answers during brief visits. National Institute on Aging outlines clear red flags you can watch for (see below).
The Signs: What You Can Observe
Even subtle changes matter. Look for patterns, not one-off events.
Physical or Medical Clues
The Department of Justice says that injuries and basic care failures are rarely “just aging.”
- Unexplained bruises, cuts, fractures, or marks suggesting restraints
- Bedsores, repeated infections, dehydration, or medication errors
- Poor hygiene, soiled clothing, or a dirty room that stays dirty between visits
Emotional and Behavioral Shifts
Distress often shows up before bruises do.
- Withdrawal, anxiety, tearfulness, sudden mood swings
- Fearfulness around specific staff or reluctance to speak with them present
- Sleep changes or new “childlike” behaviors in residents with cognitive decline
Environmental Red Flags
A troubled system leaves tracks.
- Staff dodge questions or offer changing stories
- Restricted or rushed visits, especially at odd times
- High staff turnover, visible understaffing, persistent odors, or clutter
The trauma of elder abuse can result in premature death, the deterioration of physical and psychological health, [and] devastating financial loss. — U.S. Department of Justice.
The World Health Organization’s review shows that psychological abuse is reported most often in long-term care and hospital settings.
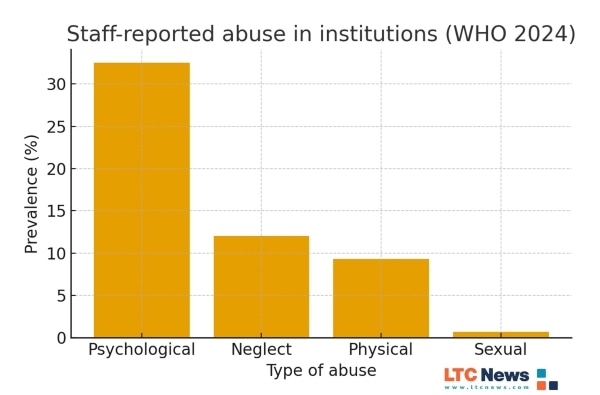
Psychological abuse includes verbal threats, humiliation, intimidation, and other nonphysical harms occur far more often than physical or sexual abuse. This type of mistreatment can be harder to detect but can leave deep emotional scars, increase anxiety and depression, and erode trust between residents and caregivers — underscoring the importance of family involvement.
Getting a Loved One to Open Up
People fear retaliation. Your goal is safety and trust.
- Find private moments. Visit at varied times and request a brief time alone.
- Ask open questions. “How are you feeling about the care here?” “Has anyone made you uncomfortable?”
- Name what you see. “I noticed a new bruise, and you seem tense when X is around.”
- Validate and reassure. “You deserve respect. I will take this seriously.”
- Document exact words. Short notes and dates matter later.
Suspect Abuse? What to Do
You do not need proof to act. If danger is imminent, call 911.
- Write it down: Dates, photos (if appropriate), names on duty, and what was said.
- Escalate inside the facility: Speak with the charge nurse and administrator; request the care plan and incident reports; note their response.
- Get an outside evaluation: Ask your loved one’s physician or a psychologist not affiliated with the facility to assess injuries or behavior changes.
- Call the Long-Term Care Ombudsman. Every U.S. state has an ombudsman who advocates for residents and can investigate complaints.
- Report to Adult Protective Services (APS): Use the Eldercare Locator (800-677-1116) to reach local APS; many states also allow online reports.
- Loop in law enforcement if crimes are suspected: For financial fraud, the National Elder Fraud Hotline is 833-372-8311 (Mon–Fri).
- Seek legal counsel. An elder-abuse attorney can preserve evidence and pursue remedies while you ensure safe placement.
Systems Can Fail but Quality Facilities Help
Your loved one’s nurses and aides are often doing heroic work. Abuse tends to rise where staffing is thin, training is weak, and leadership tolerates shortcuts. Recent reporting also shows regulators continue to penalize problem long-term care facilities — a reminder to stay involved and keep asking questions.
Finding a high-quality care facility at the outset greatly reduces risk. Even good facilities can experience problems, but you can lower the chance of harm by doing your homework. Use the LTC News Caregiver Directory to narrow your search, then visit facilities in person and talk with staff before moving your loved one in.
If your loved one has a Long-Term Care Insurance policy, the benefits will help pay for the best care in the desired setting. Get expert help filing an LTC Insurance claim. LTC News partners with Amada Senior Care to provide free claim support with no cost or obligation — File a Long-Term Care Insurance Claim.
Stay Proactive
Your involvement will deter mistreatment, so presence is protection.
Structure your routine.
- Visit often and unannounced when possible.
- Review the care plan and medication records; ask for changes in writing.
- Compare facilities using independent resources and your own eyes.
- Connect with other families to spot patterns quickly.
Trust Your Instincts — Then Act
If something feels off, it probably is. You don’t need certainty to protect someone you love. Be present, ask questions, document, and use the ombudsman/APS channels.
Your steady attention can stop harm — and spare the next resident from suffering. Elder abuse should never be tolerated. Families are already in crisis when a loved one needs extended care, and vigilance is essential.
While you work to ensure your loved one receives the highest quality care, take time to prepare for your own future needs. Explore the LTC Insurance Education Center to learn more about planning with Long-Term Care Insurance and protecting your independence as you age.


