Nursing Malpractice Puts Long-Term Care Residents at Risk

With the growing number of older adults needing long-term care services, you understand the fears and concerns. If you have a parent, spouse, or loved one in a nursing home or assisted living community, you have felt that quiet fear: What if something goes wrong when I’m not there?
It’s a real concern. Across the United States, medical errors contribute to more than 250,000 deaths each year. In long-term care settings, where residents often rely completely on nurses and aides, mistakes can be devastating.
Even more troubling, experts say that less than 10% of medical errors are ever reported, meaning the true impact on older adults may be far higher. That’s why understanding what malpractice looks like in nursing — and how it differs from simple negligence — matters for every family with someone in care.
What Nursing Malpractice Really Means
Malpractice happens when a nurse fails to meet the professional standard of care and harm results. The law requires four elements:
- Duty – a nurse-patient relationship exists.
- Breach of duty – the nurse fails to meet accepted care standards and fails to provide reasonable care.
- Causation – the breach directly causes harm.
- Damages – the patient suffers injury or loss.
Negligence, by contrast, usually involves a mistake or oversight. Malpractice is more serious — often a reckless disregard for safety. For example, a nurse who accidentally bruises a vein during a blood draw may be negligent. But a nurse who knowingly skips a protocol, causing harm, has crossed into malpractice.
Experts say that families often don’t understand the difference between a mistake or oversight and reckless disregard for safety, but for courts and regulators, intent and recklessness matter a lot.
Document Details
The Snyder Law Group, a Baltimore-based firm that has secured hundreds of millions of dollars in malpractice settlements across Maryland and Washington, D.C., said families often overlook the importance of documentation when they suspect neglect in a nursing home or assisted living facility.
Attorneys at the firm note that the first step is usually raising concerns with facility staff and observing how they respond. Families are urged to keep written records of unexplained injuries, unusual behavior changes, and the dates and times of each incident.
Those logs and conversations become vital in determining whether a facility violated the standard of care. If investigators find evidence that a nurse or provider failed to meet the accepted standard used in comparable facilities, the organization could be held liable for malpractice.
Most Common Malpractice Mistakes
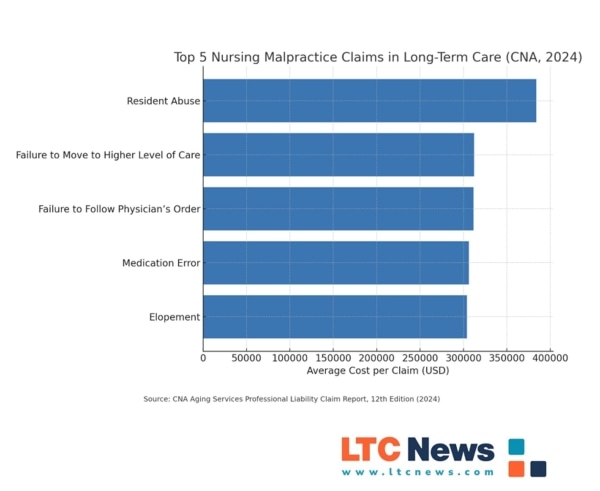
New data from the CNA Aging Services Professional Liability Report (2024) highlights the most frequent claims in long-term care:
- Falls – Nearly 41 percent of claims involve falls, with residents who have dementia especially at risk.
- Pressure injuries – Account for 22 percent of claims, often tied to inadequate repositioning or monitoring.
- Medication errors – Though less common (1.9 percent), they have some of the highest claim costs, averaging over $300,000.
- Failure to monitor – About 41 percent of cases involve staff missing vital sign changes or failing to escalate care.
- Poor communication – The Joint Commission links 80 percent of serious medical errors to miscommunication during shift handoffs.
In nursing homes, the risks are magnified. According to the Office of Inspector General (OIG), nearly one in three Medicare residents experience harm within their first 35 days of admission, with infections and medication issues leading the list.

Why System Failures Drive Nursing Malpractice
You don’t hear much about system breakdowns—but they’re often behind nursing malpractice. These aren’t just “bad nurse” stories. Your loved ones suffer when broader failures go unchecked.
Elopement (on the list above)refers to a situation where a resident of a long-term care facility — often someone with dementia or cognitive impairment — leaves a nursing home, assisted living facility, or memory care community without staff knowledge or supervision.
Workforce Cuts and Agency Chaos
Under President Trump and HHS Secretary Robert F. Kennedy Jr., HHS is undergoing a sweeping reorganization. The department announced plans to cut 20,000 jobs and merge 28 divisions into just 15 under a new umbrella, the Administration for a Healthy America (AHA).
The idea is to save money and streamline operations, but critics warn it could weaken oversight of food and drug safety, public health programs, and long-term care regulation.
Facing backlash, Kennedy acknowledged that critical services had been undermined. By late June, more than 700 CDC staffers and 220 NIH employees were rehired after their earlier dismissal.
Observers say this highlights how quickly cuts can erode the safety net that supports nursing facilities and patient protections.
What This Means for Long-Term Care
These federal changes hit close to home when you’re trusting a facility with someone you love:
- Less oversight means fewer inspections and weaker enforcement of patient-safety rules.
- Training programs suffer when agencies lose staff who support fall prevention and infection control initiatives.
- Communication lapses grow when departments are reorganized and accountability blurs.
Systemic failures like these compound the daily pressure on nursing staff:
- Understaffing and burnout – A 2023 ANA survey found 63 percent of nurses report burnout, and nearly half worry fatigue leads to errors.
- Training gaps – Poor preparation in fall prevention and medication safety leaves staff unready.
- Corporate cost-cutting – Budget-driven short staffing increases risk in both hospitals and long-term care.
- Communication breakdowns – Hierarchical workplace cultures often silence aides or LPNs who see early warning signs.
We can’t afford a system that collapses under its own weight. But we also can’t cut so deeply that patients pay the price. HHS Secretary Robert F. Kennedy Jr.
What it Means for Families
For you and your loved ones, malpractice can bring both physical and emotional fallout:
- A preventable fall leads to a broken hip, hospitalization, and permanent loss of mobility.
- A medication mistake worsens dementia symptoms or triggers organ damage.
- A missed infection forces a rushed transfer to the hospital, with lasting consequences.
Beyond the health toll, malpractice can drain savings, increase the need for higher-acuity care, and leave families reeling with guilt and anger.
Can You Protect Your Loved One?
You can’t eliminate every risk, but you can take steps to reduce them:
- Ask about staffing – What’s the nurse-to-resident ratio on nights and weekends?
- Review the care plan – Ensure it’s updated regularly and specific to your loved one’s needs.
- Watch communication – Do staff share updates clearly at shift change and with family?
- Document everything – Keep notes on changes in health, response times, and any concerns.
- Use trusted tools – The LTC News Caregiver Directory can help you compare facilities and find quality providers.
The Bigger Picture
The debate over minimum staffing rules — now tied up in federal court after being vacated in April 2025 — shows how deeply malpractice risks connect to policy. Industry groups like the Center for Medicare Advocacy argue staffing mandates are unaffordable; advocates say they could save 13,000 lives a year.
Meanwhile, families like yours are left in the middle — trying to ensure safe, compassionate care for loved ones in a system stretched to its limits.
When you trust a nursing home or assisted living facility with someone you love, you expect safety, dignity, and professional care. But malpractice remains a very real risk.
You can’t eliminate every risk. There’s no guarantee that errors and mistakes will never happen. But some long-term care facilities provide safer environments where malpractice is less likely. Those higher standards come at a price.
Quality long-term care is expensive. Medicare only pays for short-term skilled care, which means the long-term costs fall on you or your loved one unless you have Long-Term Care Insurance. Policies can cover home health aides, nurses, physical, speech and occupational therapists, adult day care centers, assisted living, memory care, and nursing home care, giving you access to better options without draining savings.
Finding safe, reliable extended care is easier when you know where to look. The LTC News Caregiver Directory connects you with vetted facilities and providers in your area. Whether you’re paying privately or relying on Long-Term Care Insurance benefits, having the right tools helps you make informed choices and protect your family.
Because while you can’t prevent every mistake, you can choose care settings that lower the risks — and give your loved one the safety, dignity, and respect they deserve.
Final Word
By knowing the warning signs, asking hard questions, and pushing for accountability, you can play a vital role in protecting your family.
Every serious case of malpractice tells us the same thing: these are preventable tragedies. Families deserve better — and residents deserve safe, quality care every day. — Nancy LeaMond, executive vice president of AARP.


