Joint Pain and Aging: How Your Body Changes and What You Can Do

Table of Contents
- What Actually Happens to Your Joints with Age
- Why Joint Pain Matters for Long-Term Care
- Everyday Habits That Protect Aging Joints
- When To Talk with a Doctor About Joint Pain
- Orthobiologics, Injections, and Joint Replacement: What You Should Know
- Joint Health, Falls, and the Cost of Extended Care
- Family Can Support Joint Health
You probably think about your heart, brain, or blood pressure when you think about aging. Your joints quietly do just as much to determine how long you stay independent.
Medical experts describe aging joints in simple terms: cartilage thins, joint fluid decreases, and surrounding muscles lose strength. Doctors say the joints become stiffer and less flexible” as you age, and cartilage can start to wear away.
That slow, steady change helps explain why arthritis and chronic joint pain are now among the leading causes of disability in older adults. Researchers estimate that one in three people over age 65 lives with osteoarthritis, the most common form of arthritis and a major driver of disability in later life.
You feel it in simple ways:
- Getting out of a chair takes more effort.
- Stairs feel harder on your knees.
- Hands feel stiff when you try to open jars or button clothing.
When pain or injury does show up, a doctor’s evaluation can help you stay mobile. Dr. Roddy McGee, a board-certified orthopedic surgeon and sports-medicine specialist in Las Vegas, notes that today’s orthopedic specialists use a wide range of options, from orthobiologic treatments to joint replacement, when conservative care is not enough.
For most adults, however, everyday habits such as movement, posture, and weight management remain the first and most important defense against long-term joint damage.
Some people ignore the problem, and if those small challenges grow, you can suddenly need help with bathing, dressing, or walking across a room. At that point, joint pain is no longer just discomfort. It becomes a long-term care problem.
What Actually Happens to Your Joints with Age
You do not have to memorize anatomy terms to understand aging joints. A basic picture helps you make better choices.
Key age-related changes include:
- Cartilage thinning. Cartilage is the smooth tissue that covers the ends of bones. With age, collagen breaks down and the surface thins and softens, which can lead to swelling and pain.
- Less joint fluid. Joint fluid acts like oil in a hinge. As you age, the volume and quality of that fluid can decrease, adding friction to movement.
- Stiffer ligaments and tendons. Connective tissues lose elasticity, so joints feel less flexible and more prone to strain.
- Muscle loss. Muscle mass and strength decline with age, placing a greater load directly on joint surfaces.
- Inflammation. Low-grade inflammation from arthritis, obesity, or other conditions can irritate joints and speed cartilage breakdown.
A 2022 CDC data brief found that about 54 percent of adults aged 75 and older have diagnosed arthritis.
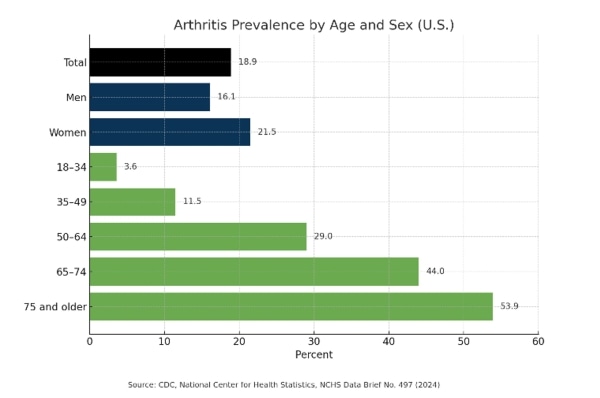
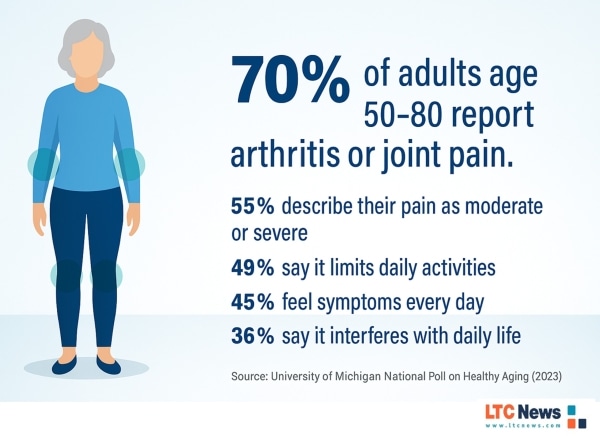
A University of Michigan National Poll on Healthy Aging reported that 70 percent of older adults say they currently experience joint pain. Those are not just numbers. They mean most people in their 60s, 70s, and 80s are making daily decisions around pain, stiffness, and mobility. In many situations, pain and limited mobility can lead someone to need help with daily living activities.
Unfortunately, that type of extended care is not covered by traditional health insurance and Medicare, which only pays for short-term skilled services. The costs and burdens of extended care will not only affect your finances but also your loved ones.
Why Joint Pain Matters for Long-Term Care
Joint pain is not only about comfort. It is closely tied to how safely you move around your home.
Large studies show that osteoarthritis, osteoporosis, and back pain often lead to limitations in basic activities of daily living (ADLs), such as bathing, dressing, and walking inside the home. Those limitations increase dependence, institutionalization, and health-care costs.
Recent research in older adults found that pain is strongly associated with difficulty in ADLs and instrumental ADLs (shopping, housework, managing medications). Pain especially affects bathing, transferring, and continence.
At the same time, federal research from the U.S. Department of Health and Human Services (HHS) shows that more than half of Americans will eventually need long-term services and supports, such as help at home, assisted living, or nursing home care.
Joint disease and pain are major reasons older adults reach that point. Aging and other chronic illnesses can complicate it even further.
So when you protect your joints today, you are not just trying to avoid tomorrow’s ache. You are lowering your odds of needing hands-on help for basic daily tasks and the high cost of long-term care later.
Everyday Habits That Protect Aging Joints
You cannot stop time. You can change how your joints age. Public health agencies and arthritis experts consistently point to the same habits:
Stay Gently, Consistently Active
Regular movement is one of the best medicines you have. The CDC notes that physical activity helps people with arthritis reduce joint pain and improve function and mood. Even moderate exercise can reduce the risk of moderate or severe functional limitations in older adults.
Joint-friendly options include:
- Brisk walking on level ground
- Water aerobics or swimming
- Stationary cycling
- Tai chi or gentle yoga for balance and flexibility
Aim for a mix of:
- Aerobic activity: 150 minutes per week of moderate activity, such as walking, broken into small chunks if needed.
- Strength training: Two or more sessions per week focusing on legs, hips, and core.
- Flexibility and balance work: Short daily sessions to keep you steady and limber.
Protect Your Joints with Smart Mechanics
Small changes in how you move can protect cartilage and reduce flare-ups.
Consider:
- Using your legs, not your back, when lifting.
- Avoiding deep squats or kneeling if they trigger pain.
- Using handrails on stairs and grab bars in bathrooms.
- Choosing chairs with firm seats and armrests so you can stand more easily.
- Manage Weight and Inflammation
Excess weight puts extra force on weight-bearing joints, especially knees and hips. Mayo Clinic and others note that higher body weight increases osteoarthritis risk through both mechanical load and inflammatory effects of fat tissue.
You do not need to reach an “ideal” number. Even modest weight loss can ease pain and improve function.
An eating pattern that focuses on:
- Vegetables, fruits, whole grains
- Lean protein and fatty fish
Healthy fats such as olive oil can support overall health and may help reduce inflammation.
Warm Up, Cool Down, And Pace Yourself
Cold, stiff joints do not like sudden demands.
Make a habit of:
- Slow marching in place, gentle leg swings, or light stretching before activity
- Cooling down with easy walking and stretches afterward
- Taking regular breaks during repetitive tasks such as gardening, cleaning, or home projects
Your goal is not perfection. Your goal is consistency.
When To Talk with a Doctor About Joint Pain
You may be tempted to brush off pain as “just getting older.” Early evaluation often prevents bigger problems.
Talk with your doctor if you notice:
- Pain that lasts more than a few weeks
- Swelling, warmth, or redness in a joint
- Joint “locking,” catching, or giving way
- Morning stiffness that lasts more than 30 minutes
- Difficulty with daily tasks such as climbing stairs, dressing, or getting into a car
Doctors may recommend:
- X-rays or other imaging to look for arthritis or injury
- Blood tests if an inflammatory or autoimmune arthritis is suspected
- Physical therapy to restore strength and range of motion
- Medication such as topical or oral anti-inflammatories, used carefully based on your health history
An article in Annals of Geriatric Medicine and Research notes that osteoarthritis is the most common form of arthritis and a leading cause of disability among older people. Delaying evaluation can allow pain and disability to snowball.
Always tell your doctor about any falls, near-falls, or sudden changes in your ability to manage ADLs. Those are red flags for long-term care planning.
Orthobiologics, Injections, and Joint Replacement: What You Should Know
Some people find that lifestyle changes, physical therapy, and standard medications are not enough. At that point, you may hear about injections or surgery.
Orthobiologics And Regenerative Options
Orthobiologics use substances from your own body (such as platelet-rich plasma or bone-marrow-derived cells) to try to reduce pain and improve joint function.
The American Academy of Orthopaedic Surgeons notes that platelet-rich plasma (PRP) is now widely used to treat pain from early knee osteoarthritis and to aid healing in certain tendon problems.
Systematic reviews suggest PRP can improve pain and function in some people with knee osteoarthritis, although study quality varies.
At the same time, major organizations point out that evidence remains mixed and protocols are not standardized. An AAOS technology overview and other reviews emphasize that current data are not strong enough to recommend PRP or other orthobiologics for every patient with arthritis.
In simple terms:
- Some patients report meaningful pain relief.
- Long-term benefits and ideal candidates are still being studied.
- Treatments can be expensive and may not be covered by insurance.
Top orthopedic surgeons offer both orthobiologic options and traditional surgery, emphasizing careful evaluation and realistic expectations.
If you consider orthobiologics, ask:
- What is the evidence for my specific condition?
- What outcomes are realistic?
- What are the costs, and is any part covered by insurance?
- What other options do I have?
Cortisone And Hyaluronic Acid Injections
Corticosteroid injections can provide short-term pain relief for some joints but may not be a long-term solution. Hyaluronic acid (gel) injections act as a lubricant in some knees and may help certain patients. Evidence for both varies by joint and severity.
Your doctor should explain:
- How often injections can be given
- Potential side effects
- How injections fit into your broader plan, not replace it
Joint Replacement Surgery
For many people with advanced joint damage, knee, hip, or shoulder replacement becomes the best option.
Modern joint replacement:
- Uses improved materials and techniques
- Often involves smaller incisions and faster rehab
- Can dramatically reduce pain and improve function in properly selected patients
Stanford Health Care notes that rheumatic diseases and advanced joint problems are leading reasons older adults lose independence, and joint replacement is often the definitive solution once conservative treatments fail.
Surgeons will look at your:
- X-rays and exam findings
- Overall health and weight
- Ability to participate in rehabilitation
- Home support and safety
Your job is to weigh risks, benefits, and your personal goals for mobility and independence.
Joint Health, Falls, and the Cost of Extended Care
You cannot control your genetics or stop every age-related change in your joints. You can stack the odds in your favor. Joint problems and falls are closely linked.
Pain and stiffness change how you walk, which can affect balance. Studies show that arthritis and chronic musculoskeletal pain increase the risk of ADL limitations, dependence, and the need for assisted living or even nursing home care.
With long-term care costs rising nationwide, being prepared has become an important part of retirement planning.
You can use the LTC News Cost of Care Calculator to see current and projected costs of:
- In-home caregivers
- Adult day care
- Assisted living
- Memory care and nursing homes
Those numbers help you see how a fall or an untreated joint problem could change your retirement budget almost overnight.
Long-Term Care Insurance will help pay for in-home help, home-safety modifications, and facility care when needed, as long as you purchase long-term care coverage before mobility and health issues become severe.
- LTC News Long-Term Care Insurance Education Center
- Compare Long-Term Care Insurance Companies and Products
Family Can Support Joint Health
You may already be helping a spouse, parent, or other loved one manage joint pain. Family support can make or break a treatment plan.
Simple actions matter:
- Offer to go along to appointments and take notes.
- Help organize home exercises and reminders.
- Encourage safe walking, not total rest.
- Watch for signs of depression or withdrawal due to pain.
When pain or mobility problems grow, the LTC News Caregiver Directory can help you locate:
- Physical therapists and rehabilitation services
- Home-care agencies with experience in arthritis and mobility issues
- Adult day centers that offer supervised exercise and socialization
Ask potential providers specific questions:
- How do you adapt care for arthritis and joint replacements?
- What training do staff receive on safe transfers and fall prevention?
- How do you involve family in goal-setting and progress updates?
If your loved one has an LTC policy, start the benefits process right away. LTC News partners with Amada Senior Care to provide free claim support with no cost or obligation. Their trained experts can walk you through the entire process and help you access benefits quickly and correctly — File a Long-Term Care Insurance Claim.
If there is no LTC policy, and your loved one has a life insurance policy, you could sell it for cash now to cover the costs of care.
You are not alone in this. Early, honest conversations about pain, safety, and future care make life easier for everyone later.
This article provides general information for adults and families and is not a substitute for personal medical advice, diagnosis, or treatment. Always talk with a qualified health-care professional about your symptoms, medications, and treatment options before making changes to your care.


