How Sleep Disorders Affect Caregivers: Strategies for Support

Table of Contents
- Why Caregivers Struggle with Sleep
- Nonprofessional Caregivers: Love and Exhaustion
- Professional Caregivers: Working Through the Night
- Recognize the Warning Signs
- Practical Strategies to Protect Your Sleep
- When to Get Professional Help
- How Sleep Problems are Diagnosed
- How Sleep Problems Are Treated
- Why This Matters for Safety and Care
- Protecting Your Health Protects Their Well-Being
- Respite Care: A Vital Lifeline for Family Caregivers
- Understanding the Cost of Care
- How Long-Term Care Insurance Fits In
You know the sound by heart — the creak of a floorboard, the cough in the next room, the quiet buzz of a monitor. It’s often enough to wake you before your body has fully rested. Some nights, you don’t really sleep at all. It is the silent toll of sleepless nights.
Being a caregiver for an older adult can mean living in a constant state of alertness. You may check on your loved one late at night or get up early to manage medications. You may lie awake listening for trouble, even when nothing happens. Over time, this takes a quiet but powerful toll on your body and your mind.
If your loved one snores loudly or has obstructive sleep apnea, it can disturb your rest every night as well as their own. Even your own stress about their health can make it hard to fall asleep when the house is quiet.
Sleep expert Dr. Michael Grandner told KCZZ radio that sleep is a biological requirement for human life. It’s non-negotiable according to experts.
We don’t sleep because we enjoy it. We don’t sleep because it’s good for you. We don’t sleep because we feel better when we do it. We sleep because actually if we don’t, we’re going to die. — Michael Grandner, PhD, Director of the Sleep and Health Research Program at the University of Arizona College of Medicine.
We do feel better when we get good sleep, and we enjoy life when we are fully rested. However, as a caregiver, you become stressed, physically, emotionally, and financially.
Caregiving is an act of love, but it shouldn’t come at the expense of your health. Sleep problems can creep in slowly, and before you know it, exhaustion becomes your new normal. That fatigue affects how you think, how you feel, and how you care.
Why Caregivers Struggle with Sleep
Caregivers aren’t just one group. Some are spouses or adult children caring for a loved one at home. Others are friends, neighbors, or unpaid family members who step in out of love and responsibility. And some are trained professional caregivers, home health aides, nursing assistants, or direct care workers who provide daily support for others.
No matter the role, caregiving can and often does disrupt normal sleep patterns and create a cycle of fatigue, stress, and declining health.
Nonprofessional Caregivers: Love and Exhaustion
If you’re a family member or friend providing care, your caregiving often doesn’t have a shift that ends. You might get up several times a night to help with:
- Toileting, personal hygiene, eating, dressing, or mobility if your loved one has limited independence
- Medication reminders or breathing equipment checks
- Monitoring symptoms and supervision for a loved one with conditions such as dementia, Parkinson’s, or other chronic illnesses
- Reassurance when confusion or anxiety spikes after dark
For many spouses, the challenges are even more personal. Sharing a bed or room with someone who snores loudly or experiences restless sleep can lead to chronic sleep deprivation. You may stay half awake listening for changes in breathing, movement, or distress. This constant state of vigilance is emotionally draining.
Research confirms what many already feel: informal caregivers, especially those living with the person they care for, experience significantly worse sleep than caregivers who live separately.
The informal caregiver also has to deal with a disrupted day–night rhythm, and that affects the carrying capacity of the informal caregiver. — 2025 study on caregiver sleep in dementia care.
A 2023 AARP and National Alliance for Caregiving report found that nearly 60 percent of family caregivers report sleep disruptions at least several nights per week, and one in three say poor sleep affects their own health. That exhaustion compounds over time, often with no formal support.
Professional Caregivers: Working Through the Night
Professional caregivers face their own set of sleep challenges. Many work long shifts, overnights, or rotating schedules, which can disrupt sleep-wake cycles and increase fatigue. Even when they’re trained to manage medical or behavioral needs, the physical and emotional demands take a toll.
- Shift work and overnight schedules lead to chronic sleep debt.
- Multiple clients or facilities mean limited time to recover between shifts.
- Emotional burnout is common, especially in dementia and end-of-life care settings.
When professional caregivers don’t get enough rest, it affects both their well-being and the quality of care they provide.
Sleep quality is directly related to general health and quality of life. Caregivers’ sleep disturbances affect not only their own health, but also the optimal care of their patients, with negative consequences such as neglect and medication errors. — A. Durak, MD, lead researcher on caregiver sleep quality study.
Recognize the Warning Signs
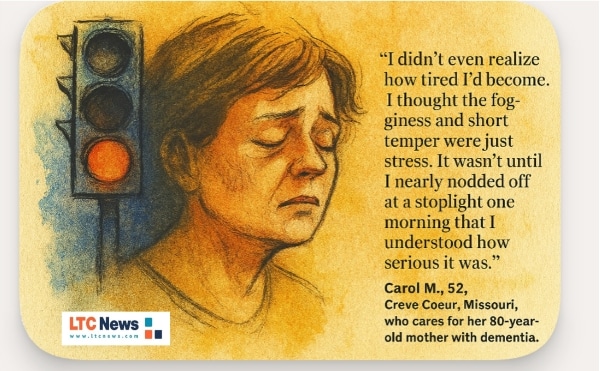
Sleep loss builds slowly, and you may not notice it at first. It starts with a few groggy mornings or snapping at someone you love when you didn’t mean to. Over time, exhaustion can become your new normal, and that’s when it gets dangerous.
You might tell yourself, “I’m just tired” or “I’ll catch up later.” But for many caregivers, “later” never comes. The signs of sleep deprivation often show up quietly before they hit hard.
Watch for red flags like:
- Feeling exhausted even after a full night of rest
- Trouble concentrating or remembering things
- Irritability or mood swings that surprise even you
- Nodding off during the day at inappropriate times, like at work or behind the wheel
h, retirement, and long-term care with LTC News —Contact LTC News.
If these symptoms sound familiar, it’s not a sign of weakness; it’s a sign your body is trying to get your attention. You can’t give what you don’t have. Recognizing these early warning signs is the first step toward protecting your health and your ability to care for someone else.
Practical Strategies to Protect Your Sleep
Small changes can make a meaningful difference over time. You may not be able to change everything about your caregiving role, but you can take steps to protect your own well-being.
Sleep specialists can offer treatments like cognitive behavioral therapy for insomnia or interventions for sleep apnea. Getting professional help can significantly improve sleep quality for caregivers (see treatments below).
Better sleep won’t erase the demands of caregiving, but it can make you steadier, more focused, and more resilient, which helps both you and your loved one.
Think of these strategies as tools, not rules. Even adopting one or two can start to ease the nightly strain. These evidence-based steps can help:
Set a Steady Routine
Go to bed and wake up at the same time every day. Your body thrives on rhythm and predictability.
Create a Sleep-Friendly Environment
Keep your room cool, dark, and quiet. Earplugs or a white noise machine can help block snoring or nighttime movement.
Address Underlying Conditions
If your loved one snores loudly or has breathing pauses, encourage a medical evaluation. Treating sleep apnea can help both of you rest better.
Recognizing that sleep and sleep disorders have an impact on the quality of a relationship could be a powerful motivator for those affected with sleep apnea to adhere to treatment. — Wendy Troxel, PhD, Senior Behavioral Scientist at RAND Corporation.
Take Short Naps
Brief naps — under 30 minutes — can boost alertness without interfering with nighttime sleep.
Share the Load
Ask family or friends to cover an occasional night. Even one uninterrupted night can help you reset.
Manage Stress Before Bed
Try five minutes of slow breathing, light stretching, or quiet reflection to help your body relax.
Limit Stimulants
Avoid late-day caffeine and be mindful of alcohol, which can fragment sleep and reduce deep rest.
When to Get Professional Help
If your sleep problems persist, talk with a healthcare provider or sleep specialist. Professional support can make a real difference. The goal isn’t just to get more hours of sleep; it’s to identify what’s interfering with your rest and treat it effectively.
How Sleep Problems are Diagnosed
Diagnosis typically starts with a conversation. Your healthcare provider may ask about your sleep schedule, stress levels, and nighttime routines. They may also screen for sleep disorders such as insomnia, obstructive sleep apnea (OSA), or restless legs syndrome.
Depending on your symptoms, they might:
- Order a sleep study (polysomnography): This test monitors breathing, heart rate, brain waves, oxygen levels, and movement overnight. It can be done in a sleep lab or sometimes at home.
- Use questionnaires or sleep diaries: These tools help identify sleep patterns, triggers, and how long symptoms have persisted.
- Check for underlying health conditions: Medical issues like thyroid problems, depression, or chronic pain can interfere with healthy sleep.
Getting an accurate diagnosis is important, especially for caregivers who may downplay their symptoms or assume exhaustion is “just part of the job.”
How Sleep Problems Are Treated
Once a diagnosis is made, treatment can begin. Options depend on the underlying cause:
- Insomnia: Cognitive behavioral therapy for insomnia (CBT-I) is the gold standard. It teaches new ways to manage thoughts and behaviors that interfere with rest, often more effectively than medication.
- Sleep apnea: Common treatments include CPAP (continuous positive airway pressure) therapy, oral appliances, or surgery to keep airways open.
- Restless legs syndrome or other movement disorders: Treatment may include medication, iron supplementation, or specific stretching exercises before bed.
- Stress and anxiety-related sleep problems: Counseling, mindfulness-based stress reduction, and relaxation training can help.
In some cases, doctors may prescribe short-term sleep medications, but most sleep experts emphasize behavioral and lifestyle changes first.
Getting treatment early can transform daily life for caregivers — boosting mood, focus, and overall health while preventing burnout.
Why This Matters for Safety and Care
Fatigue doesn’t just make you feel worn down. It can also affect your ability to provide safe, reliable care. Research shows that caregiver sleep disturbances can lead to higher stress, increased health risks, and a greater chance of errors.
The informal caregiver also has to deal with a disrupted day–night rhythm, and that affects the carrying capacity of the informal caregiver. — Huisman et al. published sleep research in 2025.
Protecting your sleep isn’t selfish. It’s part of protecting your loved one.
Protecting Your Health Protects Their Well-Being
Sleep is not a luxury. It’s fuel for your mind, body, and compassion. But here’s the truth many caregivers hesitate to admit: you can’t do this alone forever, at least not without consequences. Whether you’re an adult child caring for an aging parent or an older spouse caring for your partner, your well-being matters just as much as theirs.
Respite Care: A Vital Lifeline for Family Caregivers
If you’re providing unpaid care, respite care can give you essential breaks to rest, recover, and take care of your own health. This might mean bringing in a professional caregiver for a few hours a week, arranging adult day services, or having short-term in-home help.
Even a small amount of respite care can relieve pressure, improve sleep, and reduce burnout. Many family caregivers wait too long to ask for help, believing they “should” be able to manage on their own. In reality, using respite services is one of the best ways to keep both you and your loved one healthy and safe.
When it’s Time to Transition to Professional Care
There often comes a point where your loved one’s needs outgrow what one person, even a devoted spouse or child, can provide safely. This doesn’t mean you’ve failed. It means the level of care has changed.
Many families begin with in-home caregivers, who provide support with activities of daily living such as bathing, dressing, mobility, and medication reminders. Over time, if needs increase, families may transition to assisted living or nursing home care for round-the-clock support.
The earlier you plan for this transition, the less overwhelming it feels when the time comes. Bringing in professional help doesn’t replace your role; it supports it.
You can find professional home care providers, home health agencies, and long-term care facilities (even those that offer respite care) by searching on the LTC News Caregiver Directory. This tool allows you to search from over 80,000 providers by zip code.
If you manage a home health agency or long-term care facility you can claim your free listing on the LTC News Caregiver Directory and/or upgrade the listing to enhance visibility and highlight your staff and services through the LTC News Directory Business Portal.
Understanding the Cost of Care
The cost of paid long-term care varies widely depending on location, level of care, and setting. According to the LTC News Cost of Care Calculator, in-home care averages several thousand dollars per month or more in most parts of the U.S. Assisted living and nursing homes can cost significantly more, especially when 24/7 supervision is required.
Many families are surprised to learn that Medicare and most health insurance plans do not pay for long-term custodial care. Medicare covers short-term skilled nursing or rehab after a hospital stay, typically up to 100 days, but not ongoing daily help with personal care.
How Long-Term Care Insurance Fits In
Long-Term Care Insurance will pay for in-home caregivers, assisted living, memory care, or nursing homes, giving you or a loved one more flexibility, easing stress and burden, and protecting income and savings. An LTC policy will also cover respite care, which allows unpaid caregivers to take needed breaks without financial strain.
However, you typically can’t buy LTC Insurance once you need care. Coverage must be purchased while you’re in reasonably good health, usually in your 40s, 50s, or early 60s. That’s why early planning can make such a difference for both you and your family.
When you take the time to plan before a crisis, you preserve more than just finances; you preserve your quality of life, your family's sleep, and your relationship with the people you love.
This article provides general information and is not a substitute for professional medical advice. If you experience ongoing sleep problems or suspect a sleep disorder, consult a licensed healthcare professional.


