Parkinson’s Toll is Growing—So Are Treatment Options. Long-Term Care Services Help Improve Quality of Life

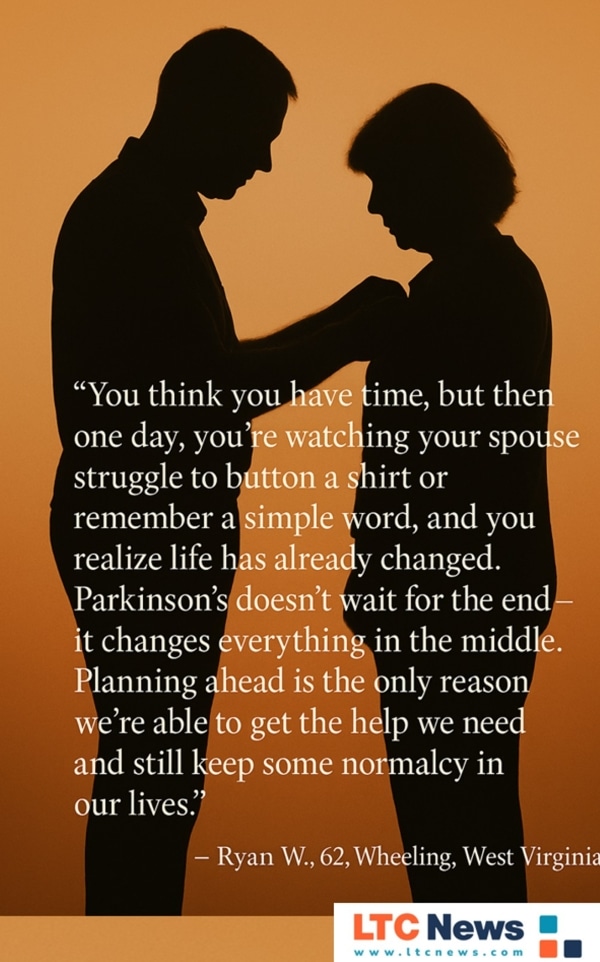
But imagine waking up one morning and realizing getting dressed, bathing, or remembering simple things is no longer easy for you or someone you love. That’s Parkinson’s today. And it’s the years, not the end, that change everything.
You might think it won’t happen to me.
But when Parkinson’s disrupts walking, talking, even thinking clearly, life shifts fast—for you and your loved ones. These are often the hardest years, not the final ones. And this is where good planning, support, and quality extended care make all the difference.
You can share your thoughts and experiences about aging, caregiving, health, and long-term care with LTC News —Contact LTC News.
Life Before Death: The Real Parkinson’s Burden
1.1 million Americans live with Parkinson’s now, and that’s set to rise to 1.2 million by 2030, according to the Parkinson’s Foundation. More than 10 million people worldwide are estimated to be living with Parkinson’s.
Parkinson’s risk rises with age, yet about 4% of cases are diagnosed before 50. Up to 70 percent eventually develop dementia, making daily life harder for individuals and their caregivers.
Activities of Daily Living (ADLs) like dressing, eating, toileting, personal hygiene, or getting around often require long-term help, and health insurance and Medicare won't pay for this extended care.
Where Parkinson’s Hits Hardest: State Mortality Data
From CDC data (2018–2022), the states with the highest Parkinson’s death rates are:
- Maine: 15.99 per 100,000 (36% above national average)
- West Virginia: 14.02
- Vermont: 13.98
New Hampshire, Florida, Nebraska, Iowa, Kansas, Minnesota, and Oregon follow in the highest mortality rates. At the low end: Alaska, at 6.44 per 100,000.
But remember—mortality stats miss the long years of disability, dementia, and dependence that families face before death.
Why Quality Long-Term Care Services Matter
Strong, adaptive programs can preserve independence, especially when long-term needs outlast skill-based healthcare coverage. Studies show multimodal rehab, combining ADL training, caregiver coaching, and home setup, boosts everyday independence and measurably reduces caregiver stress.
A former participant said of the CAPABLE program in the Washington Post, “I haven’t been to the hospital since the program. I can use my bathroom without fear.”
The extended care that many people with PD require is not paid for by Medicare or health insurance. However, those who have Long-Term Care Insurance have guaranteed tax-free benefits to pay for the extended care they need.
Those insurance benefits pay off in quality of life. A study showed that those with care paid for by a Long-Term Care Insurance policy can reduce health care utilization and costs at the end of life. These individuals see 14 percent lower overall medical costs and 35 percent fewer inpatient stays than those without it, according to the NIH study.
What Are “Strong, Adaptive Programs” for Parkinson’s?
When we talk about strong, adaptive programs in Parkinson’s care, we mean customized, evolving approaches that address the changing challenges of the disease—physically, cognitively, and emotionally.
These programs:
- Are evidence-based and proven to improve daily function and independence.
- Adapt over time as symptoms progress or new issues (like dementia) appear.
- Blend therapies so patients get comprehensive, not piecemeal, support.
Core elements include:
- Multimodal rehabilitation – Physical, occupational, and speech therapy working together to improve movement, balance, and communication.
- Activities of Daily Living (ADL) training – Techniques to help with dressing, bathing, eating, and mobility.
- Caregiver education – Training for family or professional caregivers to reduce injury risk and burnout.
- Home modifications – Adding grab bars, ramps, and adaptive equipment to keep the home safe and functional.
- Assistive technology – Mobility aids, voice amplifiers, adaptive utensils, and lift systems.
- Psychological support – Counseling, support groups, or mental health services for both patients and caregivers.
Finding Quality Care Vital to Quality of Life
It makes sense that quality in-home care can improve the quality of life of anyone who needs extended care services, including those with PD. A journal study found that programs combining ADL training, caregiver education, and home modifications significantly increased independence and reduced family caregiver stress.
At the moment, medical science can’t cure Parkinson’s, but it can dramatically improve how people live with it. With the right support, those with Parkinson’s can stay independent longer, and families cope better.
[W]e are getting better at managing the complications of the disease. Patients are living longer and better than in the past, even without any medication. — Liana Rosenthal, M.D., assistant professor of neurology at the Johns Hopkins University School of Medicine.
Fox Fighting Parkinson’s
Michael J. Fox, living with Parkinson’s since 1998, has experienced many emotions while dealing with this disease. He has said that you don’t die from Parkinson’s, but you do die with it.”
It's gettin' hard, it's gettin' harder. It's gettin' tougher. Every day it's tougher. It sucks having Parkinson’s. For some families, it’s a living hell. — actor, Michael J. Fox.
His foundation has fueled over $2 billion in research aimed at improving the quality of life for those with Parkinson's. Actor Ryan Reynolds—whose father faced Parkinson’s—said Fox “helped him feel less alone” and called him the “greatest champion of Parkinson’s research on the planet.”
Finding quality extended care can be very challenging, and paying for it, unless the care recipient has Long-Term Care Insurance, can significantly impact your family and finances.
The LTC News Caregiver Directory can make finding quality long-term care services easier. The free directory has the largest database of caregivers and long-term care facilities in the United States. You can search for providers by zip code and get the information you need to make the right decision for your loved one.
If you are a provider, you can claim your free listing on the LTC News Caregiver Directory and/or upgrade the listing to enhance visibility and highlight your staff and services through the LTC News Directory Business Portal.
If your loved one has a Long-Term Care Insurance policy, paying for the quality care they desire is much easier. LTC News partners with Amada Senior Care to help you process any LTC Insurance claim at no cost or obligation- Filing a Long-Term Care Insurance Claim.
The Coverage Gap—and Real Cost of Long-Term Care
While Medicare will pay for short-term rehabilitation, it does not cover ongoing help with daily needs such as dressing, eating, or dementia care. Yet, 58% of Americans mistakenly believe the program will pay for assisted living or in-home care, according to MarketWatch.
The reality is sobering: the annual median cost of a home health aide is about $65,757, assisted living averages $58,025 before surcharges, and a private nursing home room exceeds
$125,000, based on the LTC News survey of long-term care costs nationwide.
For families facing Parkinson’s disease, not having Long-Term Care Insurance adds to the emotional exhaustion, financial strain, and limited care choices when they are needed most. Families are often caught off guard when they discover that health insurance and Medicare do not cover extended care, and they can't purchase LTC Insurance at the time someone needs it.
Generally, people purchase an LTC policy between the ages of 47 and 67 as part of a comprehensive retirement plan. LTC Insurance is affordable, especially when using an LTC Insurance specialist who understands the product and can shop all the top-rated insurance companies that offer long-term care solutions.
LATEST TREATMENTS—Hope is Real
While Parkinson’s remains incurable, new therapies are reshaping what life with the disease can look like, offering not only symptom relief but the potential to slow its progression.
Adaptive deep brain stimulation (aDBS)
FDA-approved systems such as Medtronic’s BrainSense now deliver electrical stimulation in real time, responding to brain activity as it happens. This adaptive approach reduces symptoms while minimizing side effects. Patients report needing less medication, gaining better symptom control, and experiencing renewed daily function.
Onapgo (apomorphine infusion patch)
Approved by the FDA in early 2025, Onapgo is a wearable patch that delivers continuous dopamine under the skin. Clinical trials show it reduces “off episodes” by more than two hours a day compared with placebo, and with fewer side effects than older pump-based treatments.
Tavapadon and Vyalev
Tavapadon is an oral, once-daily D1/D5 dopamine agonist that has shown promising results in Phase III trials according to the Cleveland Clinic. Vyalev—also known as Produodopa—provides 24/7 subcutaneous delivery of carbidopa-levodopa for smoother symptom control and received FDA approval in late 2024, according to the Parkinson’s Foundation.
Prasinezumab: disease-modifying potential
This experimental antibody targets alpha-synuclein buildup, one of the key drivers of Parkinson’s pathology. Now in Phase III trials, it’s considered “at the leading edge” of treatments that aim to slow or halt progression, according to the Michael J. Fox Foundation.
Emerging drug candidates
Solengepras (CVN-424), an oral GPR6 inverse agonist, is in Phase III testing. Pirepemat (IRL-752), designed to prevent falls and improve cognition, is in Phase II trials for Parkinson’s dementia and apathy.
Stem cell therapies
Preliminary studies show that stem-cell-derived neurons can survive in the brain after transplantation and reduce tremors, raising hope for future regenerative treatments.
Psychedelic research breakthrough
A small clinical trial found that a single dose of psilocybin improved motor symptoms, mood, and memory for several weeks, without serious side effects. Larger trials are planned at UCSF. As interest in psilocybin therapy grows, so does the need for safe, supportive environments where it can be explored responsibly. Programs like psychedelic retreats, like Odyssey Retreats, that offer this kind of setting, blending guided sessions with practices that support emotional and physical well-being. While not a replacement for clinical treatment, these programs reflect a shift toward more holistic approaches to chronic illness.
Being Prepared
Parkinson’s disease reshapes life years before death, changing how families live, spend, and care for their loved one. Unfortunately, longevity brings many challenges, and the need for long-term care extends to many chronic illnesses, accidents, mobility problems, dementia, and frailty due to aging.
Quality long-term care services, started early, can protect dignity and ease burdens. Long-Term Care Insurance can provide the necessary funds to access quality care services while safeguarding assets and easing the stress on those you love.
The question isn’t if you should plan—it’s how soon you start. You can start your research by reviewing the LTC News Long-Term Care Insurance Education Center.


